Cracking the Code: Preventing Denial Code 39
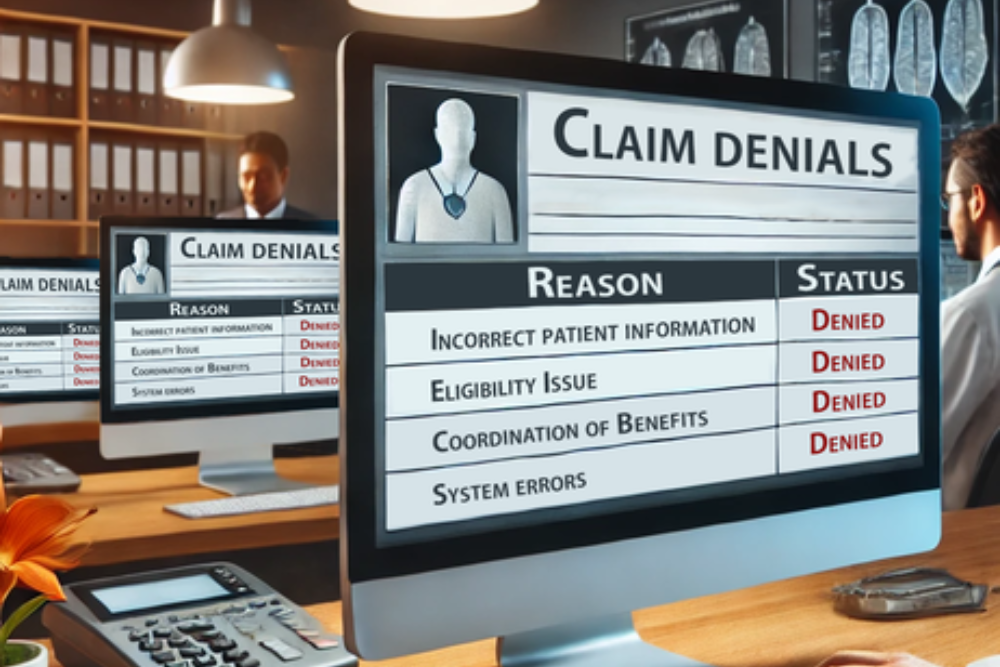
Denial Code 39, which states “Services denied at the time authorization/precertification was requested,” is a frequent challenge healthcare providers face. This denial typically arises when medical procedures are performed without obtaining the necessary prior approval from the insurance carrier. Why Does Denial Code 39 Occur?Several factors can lead to Denial Code 39, including: Strategies to […]
Cracking the Code: Preventing Denial Code 39 Read More »