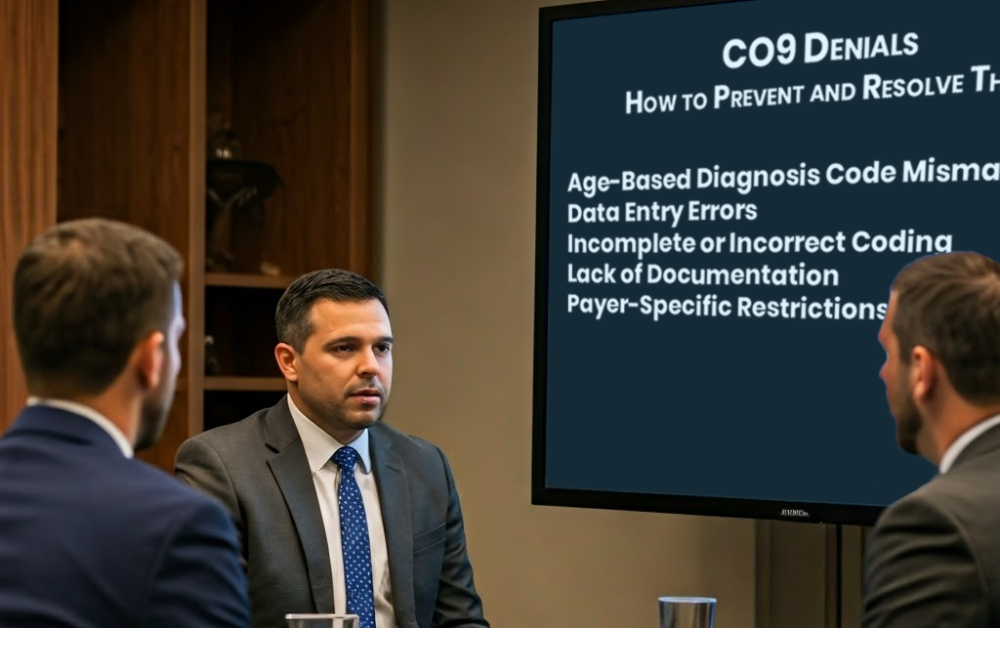
Navigate CO9 Denials: Prevention and Resolution Strategies.
CO9 denials, which result from inconsistencies between diagnosis codes and procedures, are a frequent challenge in healthcare billing. For healthcare providers, practice managers, and owners, these denials can disrupt revenue flow. This guide explains the causes, prevention strategies, and steps to resolve CO9 denials effectively. Common Causes of CO9 Denials Strategies to Prevent CO9 Denials […]
Navigate CO9 Denials: Prevention and Resolution Strategies. Read More »