CO9 denials, which result from inconsistencies between diagnosis codes and procedures, are a frequent challenge in healthcare billing. For healthcare providers, practice managers, and owners, these denials can disrupt revenue flow. This guide explains the causes, prevention strategies, and steps to resolve CO9 denials effectively.
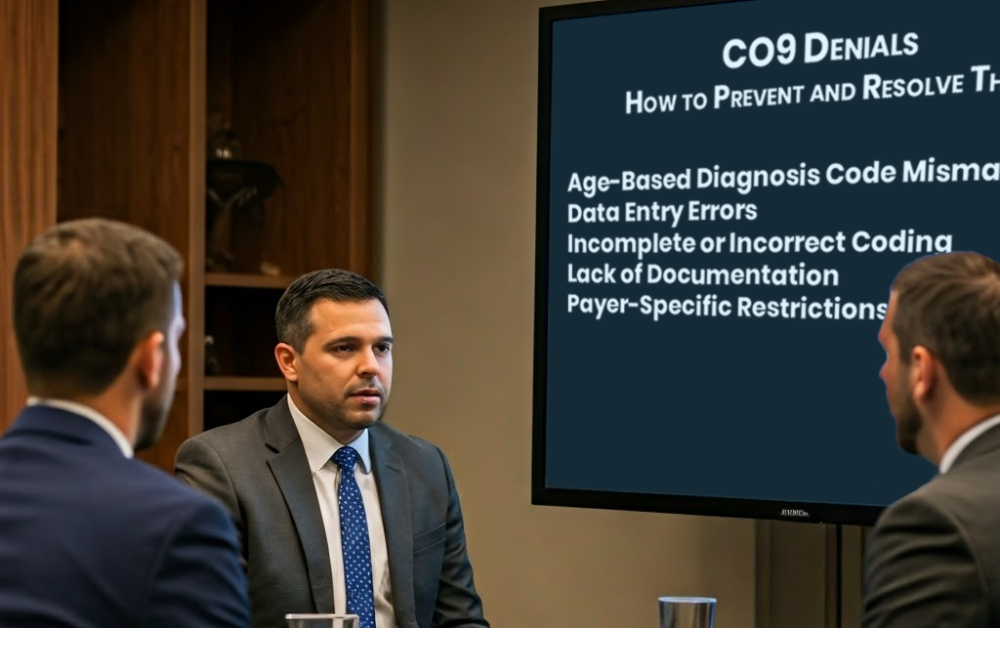
Common Causes of CO9 Denials
- Age-Based Diagnosis Code Mismatches: Using a diagnosis code unsuitable for the patient’s age (e.g., a pediatric code for an adult).
- Data Entry Errors: Mistakes like incorrect patient age or typos during billing.
- Incomplete or Incorrect Coding: Failure to apply accurate codes or required modifiers.
- Lack of Documentation: Missing medical records that validate the procedure’s necessity.
- Payer-Specific Restrictions: Overlooking payer-specific age or procedure requirements.
Strategies to Prevent CO9 Denials
- Verify Patient Age: Confirm patient demographics from reliable records.
- Ensure Coding Accuracy: Double-check diagnosis and procedure codes for consistency.
- Adhere to Payer Guidelines: Familiarize yourself with individual payer requirements.
- Review Supporting Documentation: Ensure clinical notes justify the procedure.
- Employ Technology: Leverage billing software to minimize human errors.
- Staff Training: Provide training on coding best practices and denial trends.
- Appeal Denials Promptly: Gather documentation and submit appeals to resolve denials quickly.
How Claims Med Can Help
Managing denials can be overwhelming, but Claims Med simplifies the process. With expertise in revenue cycle management, Claims Med provides tailored solutions to reduce denials and boost reimbursements. From coding audits to denial management, Claims Med helps healthcare providers achieve seamless billing operations.
Connect with Claims Med today to streamline your billing processes and resolve CO9 denials effectively!