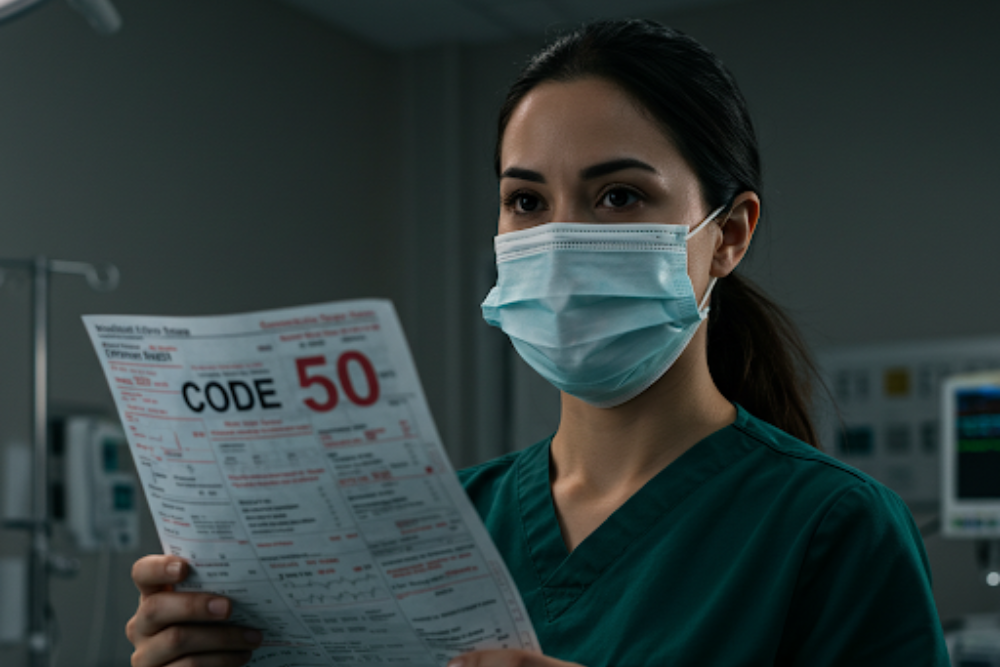
Denial code 50 is a persistent headache for practice managers, healthcare providers, and owners. It signifies that a service has been denied due to lack of medical necessity, leading to significant revenue loss. This blog explores the root causes of these denials and provides actionable strategies to improve claim acceptance rates, ensuring your practice thrives.
Understanding Medical Necessity Denials
Medical necessity is a critical criterion used by payers to determine if a service is appropriate, reasonable, and essential for a patient’s condition. When claims fail to meet these standards, denial code 50 is triggered, resulting in rejected claims and lost revenue.
Common Causes of Denial Code 50
- Insufficient Documentation: Missing or incomplete medical records, lack of supporting evidence for procedures, and vague physician notes.
- Coding Errors: Incorrect diagnosis or procedure codes that misrepresent the necessity of the service.
- Pre-authorization Oversights: Failing to obtain required pre-approval for specific services.
- Exceeding Medical Necessity: Providing services beyond what’s deemed necessary for the patient’s condition.
- Non-compliance with LCDs: Ignoring Local Coverage Determinations (LCDs) that outline specific coverage criteria.
Strategies to Combat Denial Code 50
To minimize denials and optimize revenue cycle management, implement these proven strategies:
- Comprehensive Documentation: Ensure detailed medical records, including treatment plans, progress notes, and patient outcomes.
- Accurate Coding: Double-check diagnosis and procedure codes to ensure they align with the patient’s condition and services rendered.
- Pre-authorization Compliance: Always secure pre-authorization for services requiring prior approval.
- LCD Adherence: Stay updated on LCDs and ensure all services meet payer-specific criteria.
- Streamlined Communication: Foster collaboration between clinical and billing teams to accurately reflect medical necessity in claims.
- Effective Appeals Process: Develop a robust appeals process with strong supporting documentation to challenge unjust denials.
- Patient Education: Educate patients on providing accurate and complete information during visits to avoid claim discrepancies.
Partner with Claims Med for Expert Revenue Cycle Management
Overcoming denial code 50 requires expertise and precision. At Claims Med, we specialize in revenue cycle management solutions tailored to address denial challenges head-on. Our services include denial prevention, appeals management, and claim recovery, helping you:
- Increase claim acceptance rates
- Improve cash flow
- Enhance practice efficiency
Don’t let denial code 50 drain your revenue. Contact Claims Med today to transform your revenue cycle and secure your practice’s financial health.